It’s 2014, which means the bulk of the Affordable Care Act is now in effect. While most of the mainstream media has focused on whether patients will finally be able to find affordable health insurance through the programs it creates (or not), very little attention has been paid to discussing how the wide-ranging law is being capitalized upon by healthcare corporations, and how some of its other incentives and provisions change the registered nurse’s scope of practice, speed up the computerization of healthcare, and encourage fundamental changes to healthcare delivery and systems. In fact, these changes are redefining the meaning of “care” that healthcare providers, like you, are expected to provide.
Registered nurses do not need to know every minute aspect of the Affordable Care Act, but they should understand in general what goals the legislation claims to set and the kinds of problems it claims to solve.
U.S. healthcare policymakers often can’t agree on much, but the one thing almost all agree on is that the United States spends way too much money per capita per year on healthcare, about $8,508 according to the Organization for Economic Cooperation and Development. It’s the highest of all countries in the world. But for that price tag, we get less-than-stellar results. Our infant mortality and longevity rates are far behind all other Western, developed nations.
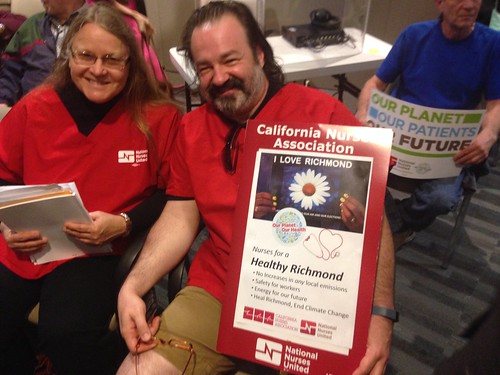
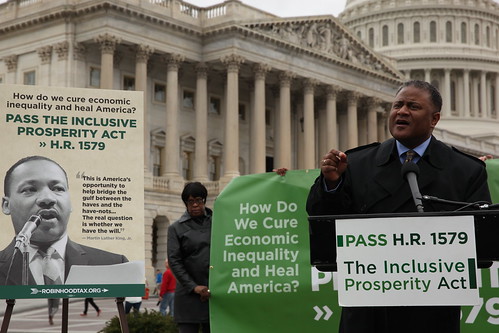
National Nurses United has long argued that to lower our expenditure on healthcare and promote a single, high standard of good care, we need to remove the profit motive from healthcare and run it like the public utility that it really should be. All people need things like clean water, electricity, police and fire rescue. These services are critical to sustaining human life. Accordingly, we often operate the systems that provide these services as a public entity, for the public good and not for profit.
It should be the same with healthcare. All people have bodies. We all fall sick, have babies, grow old, get into accidents, sustain injuries, die. For this reason, NNU has long advocated for, at the very least, a single-payer health insurance system that covers everybody from birth to death and is funded by everyone’s tax dollars. That’s how most other industrialized countries have set up their healthcare financing systems. They don’t run healthcare as a business or view healthcare as an appropriate arena in which to make profit.
The United States, on the other hand, continues to let healthcare corporations call all the shots. That’s why, when we examine the Affordable Care Act, which was crafted with the help of companies such as Kaiser Permanente and Pfizer, we see a law that does not at all challenge the dominance of healthcare corporations and actually facilitates their ability to make money by enabling the least, cheapest, and fastest care possible.
The law aims to “improve quality” and “increase value” by supposedly promoting greater coordination between doctors, hospitals, and insurance companies by merging them into one entity; relying on healthcare information technology to limit care options by ensuring adherence to “evidence-based care;” and encouraging institutions to give care in settings outside of the hospital (cheaper settings) with lesser-trained and skilled providers (cheaper labor).
Guess what? These are all goals that the healthcare industry had anyway. The ACA codified some of these aspirations, turning them into the law of the land.
Now that the dust has settled around healthcare reform, corporations are redoubling their efforts and accelerating the race to the bottom. Almost all hospitals across the country are adapting and attempting to transform themselves in a way that takes full financial advantage of the current system. Sometimes it means merging with bigger, corporate chains and sometimes it means buying up those smaller community hospitals. But, increasingly, it also means that registered nurses are noticing their employers venturing into activities like opening up urgent care clinics around town and setting up their own insurance plans – on top of continuing to make the relentless cuts to services, staffing, equipment, and supplies that they always have. Here at National Nurses United, we often refer to all of these changes as healthcare “restructuring.”
In this article, we will list the top five trends RNs must know about this restructuring. Since the bottom line of all this reorganization is always to make more money, a goal that is typically in conflict with our role as patient advocates, registered nurses must work together at the unit level, facility level, and organizational level to fight any changes that would harm our patients or our practice. But, as always, the first step is education, so read up.
1. Hospitals will use the Affordable Care Act as an excuse for anything and everything horrible they want to do
It’s like the 2014 hospital version of “The dog ate my homework.” Want to cut benefits for part-time RNs? It’s because of the ACA. Want to make layoffs? Blame the ACA. Want to reduce the hours for per diem nurses? The ACA made us do it. As soon as it was signed into law in 2010, hospitals started using the law and the “uncertainty” and “ambiguity” it supposedly created to justify all types of changes, mainly cuts to services and staffing. The ACA has been invoked at multiple bargaining tables, including Sutter Health and Kaiser Permanente, usually as the basis for some type of argument that the hospital will collect less revenue through drops in reimbursement. Hospitals never seem to anticipate that their revenue will rise due to the increased number of people eligible for Medicaid and who will now carry health insurance.
2. Hospitals are trying to shift patients who need to be in the hospital out of the hospital
Yes, hospital care can be expensive, but that’s largely because hospitals charge so much (See page 6 for report on excessive hospital charges), plus money gets siphoned away to fund million-dollar executive pay packages, advertising and marketing campaigns, and profits to shareholders. To rein in spending, the ACA encourages care to be provided in non-hospital settings. This means several things, including figuring out ways to move patients through the hospital faster, discharge patients early, or never admitting them into the hospital in the first place. In the Kaiser Permanente system, nurses are seeing patients held under “observation” status without formal admission for up to 24 hours before being sent home, and also changes in treatment protocols that shift care to outpatient settings or the patient’s home. There, the burden of care is put on sometimes very ill patients themselves or on their family members. For example, a Kaiser facility in California’s Central Valley used to admit patients with deep vein thrombosis so that providers could administer blood thinners and monitor patients to make sure their clots did not cause more problems, but Kaiser protocols have changed in the past couple of years so that RNs are told to teach patients or their relatives how to inject themselves and to return every day for testing of clotting levels.
Clinic care does have its role in the healthcare system, agree RNs, but patients who legitimately require the type of round-the-clock observation and care RNs can provide in a hospital should not be shunted into a 15-minute clinic visit.
Not surprisingly, some hospitals are rapidly building new clinics. Kaiser is apparently experimenting in constructing clinics with prefabricated walls, with the first such building in Kona, Hawaii. According to a June 2013 West Hawaii Today article, a team manager for Kaiser’s National Facilities Services described the Kona clinic as a “pilot project” and that “national Kaiser officials wanted to find a way to make building clinics ‘faster, better (and) cheaper.’”
RNs point out that clinics are often staffed by lesser-skilled and nonunion workers and more loosely regulated. For example, the mandatory RN-to-patients ratios law that sets a maximum number of patients per nurse does not yet apply to clinic settings.
3. Everyone wants to violate your RN scope of practice
You, my dear RN, are a highly educated, trained, and skilled healthcare provider. Your labor does not, and rightly should not, come cheap. But the healthcare industry, anticipating many millions more people accessing healthcare, wants that care to be provided most “efficiently” (read: at the lowest cost possible). At the same time, industry-connected policy wonks complain about a lack of RNs and general practitioners to provide the primary and preventive care people need. Instead of investing in the education of more registered nurses, nurse practitioners, and medical doctors (many countries provide a free or heavily subsidized medical school education), they argue that healthcare should be delivered “in new ways.”
That’s why, across the country, there is a huge push for all kinds of lower-skilled, unlicensed staff to assume registered nursing duties and practice, and to dissect and break down the complex work that RNs do into discrete tasks to be parceled out to ancillary staff.
In California, Minnesota, Michigan, as well as other states, hospitals and other healthcare policy organizations are lobbying for medical assistants, paramedics, emergency medical technicians (EMTs), and licensed vocational or practical nurses to take on expanded roles. For example, in a July 2013 white paper, the UC Davis Institute for Population Health Improvement recommended that California launch pilot programs in which paramedics who received additional training get to assess whether patients need to be transported to an emergency department or should be treated by the paramedic as needed; to essentially serve as home health RNs to follow up on patients who had been discharged from the hospital; and to provide care for patients with chronic conditions.
In one “Challenges” section of the paper, the authors write that “patients may perceive there are tiers of care or lower levels of care being provided by the [community paramedic] if the patient is accustomed to receiving care from doctors or nurses.” They’re right to worry, because it’s true; this program does create inferior levels of care.
In Michigan last November, Sparrow Health System replaced all the registered nurses at its urgent care clinics with unlicensed medical assistants, though nurses warned that this move was bad for patients. “Patients who walk into an urgent care should be assessed by a highly trained RN who can detect serious problems that may go unnoticed to an untrained eye,” said Jeff Breslin, RN and president of the nurses union at Sparrow. “Registered nurses have the skills and experience to tell immediately whether patients need more advanced care.”
At San Joaquin General Hospital in French Camp, Calif., nurses objected last year when the hospital wanted medical assistants in its ambulatory care clinics to provide services such as diabetic foot screens. Management expected medical assistants, who in California are not licensed nor even certified by any medical board or body, to fill out a sheet that asked them to answer questions such as, “Has there been a change in the foot since last evaluation?” and “Is there a foot ulcer now or history of foot ulcer?” and “Does the foot have an abnormal shape?” The nurses had also obtained a copy of a separate “skills academy” form that supposedly recorded which in a long list of “skills” the outpatient clinic assistant (medical assistant) had received training in. These “skills” ranged from the diabetic foot exam just mentioned to staple and suture removal and “anticipating needs” for patients who complained of chest or abdominal pain. The RNs believe that these evaluations constitute nursing assessment and should be performed by a registered nurse, not a medical assistant, and are currently working on correcting this problem.
These are all examples of how care by registered nurses is being split into simpler tasks that can then be parceled out to unlicensed personnel to complete. What’s missing in this new model of medical care is a fundamental appreciation of how registered nurses are not educated, trained, and experienced to only just perform medical tasks, but to contextualize and synthesize all the information they collect to provide an individualized assessment of any particular patient. Nurses use that assessment to make ongoing judgments or decisions about the best course of therapy or treatment for that patient.
Healthcare corporations who are attempting to break down nursing care into its constituent parts fail to understand that the sum of the parts does not equal the whole – or perhaps they do know but do not care. For the sake of their patients and their own profession, registered nurses must fight to protect their scope of practice and force them to care.
“Hospitals continue to shop around for a cheaper way of delivering care to patients, but it doesn’t work,” said Karen Higgins, RN and a member of the NNU Council of Presidents. “They’ve tried it before. It’s never worked, and it puts patients at risk. You need to have a good, educated, experienced registered nurse.”
4. Hospitals will be accelerating rollouts of dangerous electronic health records systems
Any RN who has experience with electronic health records systems (EHRs), whether they be electronic charting, electronic medication administration, pharmacy programs, or computerized physician order entry, knows that they do not support or complement nursing care. It’s obvious to RNs that there is little nursing value in being forced to stand in front of a screen and click a bunch of little check-off boxes or select from pages and pages of drop-down menus.
Instead, EHRs exist to help the hospital make more money by maximizing billing for every item or service the patient uses unless, like Kaiser, the hospital is paid a flat fee for treatment. In that case, the hospital may use EHRs to limit the amount of care provided. Under any business model, EHRs also maximize earnings by limiting healthcare providers’ use of independent judgment in treatment options.
Built into these electronic health records systems is what’s called clinical decision support software, which is just a fancy name for software code that prompts the user to adopt whatever treatment plan the computer thinks is appropriate based on a fictitious, “average” patient in its database. This is the software programming that, for example, limits the choices you can check off when you are trying to chart or makes a pop-up warning window appear on your screen that you have to override if you want to continue. If this sounds like the computer is taking over your independent nursing judgment and maybe ultimately your job, that’s because it is.
Electronic health records systems seek to routinize and standardize care. Not only is this cheaper, but it’s simpler and easier and can be done by non-registered nurses in non-hospital settings. There’s less variation, everyone gets the same thing, care is not individualized. Again, there’s less and less independent judgment involved, which is exactly what registered nurses excel at: applying their knowledge and experience to make decisions in unexpected situations. Human bodies are not inanimate widgets; they are complex systems and some may behave and respond differently than others to the same drugs, treatments, or procedures. Patients need registered nurses to help figure out and advocate for the type of care that particular patient needs, not what the computer thinks is best.
Additionally, EHRs are a critical foundation upon which all types of remote care can be implemented, whether it’s electronic intensive care units where doctors and RNs are watching patients 100 miles away via video cameras, video conference medical examinations, or virtual diabetes management clinics where patients use home sensor devices to transmit data and vitals to the computer system. EHRs not only enable healthcare corporations to shift care out of the hospital, but ultimately remove people – face-to-face contact – from healthcare.
“Care tools will be on site in many people’s homes,” reads a 2012 slideshow presentation titled “Kaiser Permanente’s Healthcare IT Journey” by the company’s then-CEO, George Halvorson. “Some…technology for in-home care two years from now will be as good or better than actual hospital inpatient technology was five years ago. In-home monitoring, EKGs, ultrasounds, video conferences, blood and fluid diagnostic and testing tools will be increasingly sophisticated, effective, and cheap.”
What’s missing from this picture? That’s right, you.
And, by the way, the federal stimulus package passed in 2009 incentivizes the adoption of electronic health record systems – what is often termed “meaningful use” – through subsidies and penalties. It included massive incentive payments, about $30 billion, for hospitals that can demonstrate that their electronic health record systems work with computerized physician order entry (CPOE) and clinical decision support systems. Beginning in 2015, some hospitals may face reduced Medicare reimbursements for failure to adopt EHRs.
5. Hospitals are turning into insurance companies AND doctors’ groups
Instead of eliminating the root cause of our outrageous healthcare costs, the profit motive, the Affordable Care Act operates from the assumption that costs can be brought down if only hospitals, doctors, and insurance companies better coordinated and cooperated with one another over care and reimbursements. The ACA promotes the creation of accountable care organizations, which are essentially “integrated” healthcare systems like Kaiser Permanente, where the hospital not only owns and runs the hospital, but acts as the insurance company as well as hires and pays the doctors. If an accountable care organization meets certain so-called quality standards such as patient satisfaction and saves money at the same time, it is allowed to keep a share of those savings.
RNs are concerned that this type of power dynamic incentivizes these ACOs to deny care, since they will be able to pocket more of the insurance premiums as well as control what physicians and nurses can and cannot provide as treatment. “Absolutely there’s a conflict of interest,” said Jean Ross, RN and a member of the NNU Council of Presidents. “Independent judgment, I think, is quashed.”
If Kaiser is the model, we should all be very, very worried, say RNs. Kaiser has advanced further in all of the trends than most employers. Currently, nurses who work for Kaiser are fighting what they see as a deliberate push by the healthcare giant to keep patients who need hospital care out of the hospital by discharging patients early or sending patients to clinics staffed mostly with medical assistants or simply just home. It then claims that because of reduced hospital census, it needs to lay off registered nurses and cuts remaining staff to the bone. According to a January 2013 Los Angeles Times article, Kaiser has captured 40 percent of California’s health insurance market, and nearly one out of every five Californians is a Kaiser member, according to Kaiser membership and state population figures.
“Currently, the Kaiser model of care is becoming one of denying care,” said Katy Roemer, an RN nurse rep leader in the Kaiser system. “That way they can pocket more of the premiums. When you subject healthcare to the business model, this is where you’re going to end up. As nurses, we’re here to take care of patients. Anything that gets in the way of us being able to take care of our patients, we are going to fight.”